Ever wondered why recovery feels like a slow climb up a steep hill? Here’s a twist: Compression socks after surgery could be the secret gear you’re missing in your post-op toolkit. Imagine speeding up your healing process, all while reducing discomfort and swelling. Sounds too good to be true? Dive into our guide, and let’s unravel the science behind these snug wonders. We’ve got all the answers to your burning questions, ensuring you’re not just stepping towards recovery—you’re leaping.
Get ready to embrace a smoother, more comfortable recovery journey.
What Are Compression Socks After Surgery?
After surgery, your body embarks on a journey of healing and recovery. During this time, managing swelling and reducing the risk of complications like blood clots are top priorities. This is where compression socks come into play. Designed to apply gentle pressure to your legs, these socks promote blood flow, aiding in quicker, more efficient healing. They’re not your average socks; think of them as your personal health assistants, working tirelessly to keep your circulation in check.
Compression socks for post-surgery use are engineered with specific materials and graduated pressure levels to ensure optimal support for your recovery. Whether you’ve had elective surgery on your legs, abdomen, or even cosmetic procedures, these socks serve a crucial role in your healing arsenal. By squeezing your legs gently, they help blood vessels work better: the arteries that take oxygen-rich blood to your muscles can relax, allowing blood to flow freely. The veins get a boost pushing blood back to your heart.

Here’s a quick scan of why they’re essential:
- Enhanced Blood Circulation: Promotes the flow of blood back to the heart.
- Reduced Swelling: Minimizes fluid buildup in the legs.
- Prevention of Blood Clots: Lowers the risk of deep vein thrombosis (DVT), especially after major surgery when you’re less active.
Embracing compression socks post-surgery can significantly affect your recovery trajectory, making it smoother and more comfortable. Let’s dive deeper into how these socks can help you bounce back stronger.
Do Compression Socks Help Recovery?
Compression stockings prevent blood clots from forming in your veins when you sit or stand for longer periods of time. This issue has been observed in people above 50 or people who have low blood pressure issues. If you want to improve blood flow in your legs, consult your doctor and use compression therapy or wear graduated compression socks.
Yes, and here’s how they turn the tide in your favor. After surgery, your body is in a delicate state, focusing all its energy on healing. Being inactive or confined to a bed can slow down blood circulation, which is where compression socks shine. They’re like a gentle, constant massage for your legs, keeping blood moving and reducing the risk of complications that could set your recovery back.
Source: https://www.gethealthyveins.com/
Key Benefits
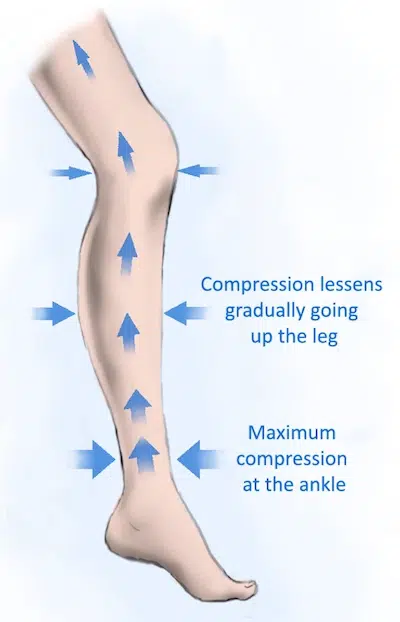
- Swelling Reduction: By applying graduated pressure from the ankle upward, compression socks effectively combat swelling, a common post-surgery complaint. This not only feels more comfortable but also aids in faster recovery.
- Prevention of Varicose Veins: Regular use of compression socks can help prevent the formation of varicose veins, which are more likely when your mobility is limited during recovery.
- Enhanced Circulation: Improved blood flow means more oxygen and nutrients are delivered to your muscles, speeding up the healing process.
- Lowered Risk of Blood Clots: Stagnant blood flow can lead to dangerous clots. Compression socks reduce this risk by keeping blood circulating.
Scientific Backing
Studies support the use of compression socks for post-surgical recovery. One study found that patients who wore compression socks after surgery had a significantly lower risk of developing DVT compared to those who did not.
User Experiences
Many patients report feeling less pain and swelling when wearing compression socks as part of their recovery regimen. The comfort and security they provide can also offer peace of mind during a stressful recovery period.
Incorporating compression socks into your post-surgery care plan can significantly enhance your recovery process. They’re a simple, non-invasive tool that brings a host of benefits to the table.
What Type of Compression Socks Are Best After Surgery?
Choosing the right compression socks after surgery is crucial for your recovery. The market is flooded with options, but not all are created equal when it comes to post-surgical care. Let’s break down what you need to consider to find your perfect pair.

Material Matters
Look for socks made from breathable, skin-friendly materials. Comfort is key, especially when you’re wearing them for extended periods. Fabrics that wick away moisture can also prevent irritation and skin infections.
Graduated Compression
The best compression socks for you depend on your individual needs, including the type of surgery you had, your risk factors for blood clots, and your personal comfort preferences. Always consult with your healthcare provider before making a decision.
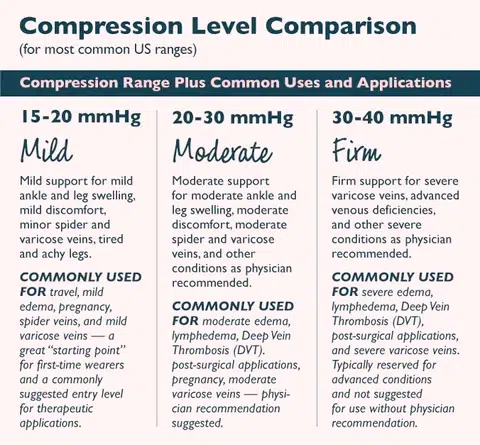
Compression Level
Compression socks come in various pressure levels, measured in mmHg (millimeters of mercury). For post-surgical recovery, light to moderate compression levels, typically between 15-30 mmHg, are often recommended. However, your healthcare provider should be your go-to for advice on the exact level needed for your specific situation.
Source: https://www.rejuvahealth.com/
Size and Fit
Getting the right size is essential. Too tight, and you are at moderate or high risk of cutting off circulation; too loose, and you won’t receive the benefits of mild compression. Many brands offer a sizing chart based on your shoe size and calf circumference. A proper fit ensures maximum effectiveness and comfort.
Length
Knee-high compression socks are generally recommended for post-surgical recovery. They target the area most prone to swelling and clotting without being as restrictive as thigh-high socks. However, your doctor may recommend a different length based on your surgery or medical history.
Top Picks
While specific brand recommendations can vary, looking for those with high user ratings and positive reviews within the medical community can guide you to a quality purchase.
The best compression socks for you depend on your individual needs, including the type of surgery you had, your risk factors for blood clots, and your personal comfort preferences. Always consult with your healthcare provider before making a decision.

How Long Do I Really Need to Wear Compression Socks After Surgery?
The duration for wearing compression socks post-surgery is as unique as your recovery journey. Generally, healthcare providers recommend wearing them for at least two weeks after surgery. However, this period can extend to several weeks or months, depending on factors like the type of surgery you had, your mobility level, and your risk of developing blood clots.
Guidelines to Consider:
- Follow Your Doctor’s Advice: Your healthcare provider will give you tailored advice based on your specific circumstances.
- Monitor Your Recovery: The better and quicker your mobility improves, the less you may need to rely on compression socks.
- Risk of Blood Clots: If you have a higher risk of DVT, you might need to wear them longer.
Remember, wearing compression socks is part of your recovery, not the entirety. Combine their use with other doctor-recommended practices like gentle exercises and staying hydrated.

How Many Hours a Day Should You Wear Compression Stockings?
For optimal results, aim to wear your compression socks for most of the day. Putting them on in the morning before you get out of bed and taking them off before bed is a good routine. This schedule helps prevent blood from pooling in your legs when you’re most active.
Exceptions & Adjustments:
- During Sleep: You typically don’t need to wear them unless advised by your doctor.
- Listen to Your Body: If you experience discomfort or any adverse effects, consult your healthcare provider.
It’s all about balance. Wearing compression socks should feel supportive, not restrictive. Adjust as needed, and always prioritize comfort along with efficacy.
Should You Wear Compression Socks at Night?

While compression socks are beneficial during the day, wearing them at night is usually unnecessary. When you’re lying down, your legs are on the same level as your heart, which naturally improves blood flow and reduces swelling.
Key Points:
- Risk of Circulation Restriction: Prolonged compression while inactive could potentially restrict circulation if the socks are too tight.
- Comfort and Skin Health: Allowing your skin to breathe and recover from the pressure during the day helps maintain healthy skin.
Exceptions exist, and in certain cases, your doctor might recommend nighttime wear. However, for most people, giving your legs a break at night supports both comfort and circulation.
When Should You Not Wear Compression Stockings?
Compression stockings are a boon for many in recovery, but they’re not for everyone. Understanding when to skip them is crucial for your health and comfort.
Specific Conditions to Consider
- Peripheral Neuropathy or Diabetes: If you have reduced sensation in your legs, graduated compression stockings might cause unnoticed injuries.
- Peripheral Arterial Disease (PAD): For those with PAD, compression can worsen the condition by further restricting blood flow to the limbs.
- Skin Infections or Open Wounds: Wearing a compression stocking over affected areas can hinder healing and exacerbate issues.
- Severe Dermatitis or Allergic Reactions to Material: If the material irritates your skin, it’s best to avoid use.
Always consult with your healthcare provider to determine if compression stockings are safe for your specific health conditions.
How Long After Surgery Are You at Risk for Blood Clots?
The risk of developing blood clots, particularly deep vein thrombosis (DVT), remains heightened for weeks or even months after surgery. The exact duration depends on factors like the type of surgery, your mobility level, and your overall health.

Source: https://www.westernvascular.com/posts/what-is-a-deep-vein-thrombosis/
Risk Timeline
- Immediate Post-Surgery Period: The first 10 to 14 days are critical, as your activity level is usually reduced.
- Extended Risk: Depending on your surgery type and personal health history, the elevated risk can last for up to three months or more.
Preventive Measures
- Wearing compression stockings as directed.
- Gradually increase physical activity as recommended by your healthcare provider.
- Staying hydrated and following a healthy diet.
Awareness and proactive measures are key to minimizing your risk. Your healthcare team will guide you through the best practices for your situation.
Can Compression Stockings Dislodge a Clot?
A common concern is whether compression stockings might cause an existing blood clot to break loose and travel to dangerous areas, like the lungs. The reality is, when used correctly under medical supervision, compression stockings significantly reduce the risk of DVT or pulmonary embolism, but are unlikely to dislodge an existing clot.

Compression stockings prevent blood clots from forming in your veins when you sit or stand for longer periods of time. This issue has been observed in people above 50 or people who have low blood pressure issues. If you want to improve blood flow in your legs, consult your doctor and use compression therapy or wear graduated compression socks.
Understanding the Safety
- Graduated Compression: These socks are designed to apply pressure in a way that supports blood flow toward the heart without exerting undue force on the clot itself.
- Medical Supervision: Before prescribing compression stockings, doctors evaluate the risk of DVT and ensure the stockings complement your specific treatment plan.
Research Insights: Studies have shown that compression stockings, when part of a comprehensive post-surgery care plan, can help prevent blood clots without dislodging existing ones. They are a preventive measure, not a treatment for existing DVT.
Bottom Line: If you have a history of blood clots or are concerned about DVT, it’s crucial to discuss with your healthcare provider whether compression stockings are appropriate for you. They can assess your situation and recommend the best course of action.
Step Confidently into Your Recovery With Compression Socks
You’ve just navigated through the essentials of how compression socks work for post-surgery recovery, arming yourself with knowledge to enhance your healing journey.
Let’s quickly recap the highlights, ensuring you’re fully equipped to make informed decisions:
- Graduated compression is key for effective recovery.
- Choose the right material and fit for maximum comfort.
- Consult with your healthcare provider for personalized guidance.
- Understand when to wear them and when to give your legs a break.
Compression socks are more than just a recovery tool; they’re a step towards reclaiming your mobility and freedom after surgery. With the right pair, you can accelerate your healing process, feeling more like yourself every day.
FAQs about Compression Socks After Surgery
1. How long do you need to wear compression socks after surgery?
Generally, healthcare providers recommend wearing them for at least two weeks after surgery. However, this period can extend to several weeks or months, depending on factors like the type of surgery you had, your mobility level, and your risk of developing blood clots.
2. What are the benefits of compression socks after surgery?
- Enhanced Blood Circulation: Promotes the flow of blood back to the heart.
- Reduced Swelling: Minimizes fluid buildup in the legs.
- Prevention of Blood Clots: Lowers the risk of deep vein thrombosis (DVT), especially after major surgery when you’re less active.



